Women’s issues have historically been ignored in spinal cord injury (SCI) research, and limited attention has been given to exploring gender differences in physical and psychological health following SCI. With women composing about 19% of people with SCI (NSCISC, 2012), most research understandably has been based predominantly on samples of men. Existing literature documents high rates of depression and psychological morbidity following SCI, with one recent study finding the rate of probable major depression three times higher in people with SCI than in the general population (Fann et al., 2011). Rates of depression are consistently higher among women than men in the general literature; however, given the paucity of research on women with SCI, it is unclear whether rates of depression are actually higher among women than men with SCI. With limited comparative data on which to make definitive conclusions, recently published literature reviews on the psychological health of people with SCI (Craig et al., 2009; Post et al., 2012) have ignored the obvious question of gender differences. While early studies seemed to confirm findings from the general population that depression is more prevalent among women than men with SCI (Hughes et al., 2001; Krause et al., 2000), more recent findings have been mixed, with some studies reporting poorer psychological health among women (Arango-Lasprilla, 2011; Fann et al., 2011; Krause et al., 2004; Krause et al., 2007) and others finding no differences in psychological health and morbidity between men and women with SCI (Kalpakjian et al., 2006; Woolrich et al., 2006).
| Examples of Common Symptoms of Depression | |
| Non-somatic Symptoms | Somatic Symptoms |
| Loss of Pleasure | Loss of Energy |
| Feelings of Worthlessness | Changes in Sleep |
| Loss of Interest | Changes in Appetite |
| Irritability | Tiredness or Fatigue |
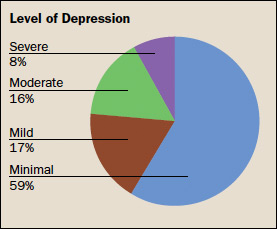
As researchers at the TIRR Memorial Hermann Spinal Cord Injury and Disability Research Center (SCIDR), we are committed to understanding the experiences of women with SCI and other disabilities and addressing their unique issues and needs. In a recent study of women with a broad range of physical disabilities (Robinson-Whelen et al., 2013), we found that depression was a significant issue for many of the women in our sample, with more than half of the women classified as experiencing significant symptoms of depression. Most promising in this study, we found that the strongest predictors of depression were factors that may be modifiable with interventions designed to improve pain management and enhance social networks.
In a second study specifically examining depression among women with SCI (Robinson-Whelen et al., 2014), we again found rates of depression to be high, with a third of the women experiencing depressive symptoms that were indicative of clinical depression. Particularly concerning was the finding that the majority of the women with elevated depression scores had not received any treatment for depression in the past three months. An examination of both recent and lifetime depression treatment revealed a pattern of predominantly pharmacologic treatment of depression and depressive symptoms, with very few women receiving any counseling or psychotherapy services for their depression. In this study, depression among women with SCI appeared to be underdiagnosed and undertreated.
One challenge in diagnosing depression among people with SCI or chronic disabling health conditions is the availability of valid measures of depression. Most measures of depression contain items that assess somatic symptoms of depression, such as lack of energy and sleep disturbance. There has been controversy about whether or not such measures are valid for use in populations with significant physical health issues when the somatic symptoms of depression and the underlying disability or health condition could be confounded. With our collaborators, we have recently examined one such widely used measure of depression, the Beck Depression Inventory-II (Beck, Steer, & Brown, 1996). Our findings support the reliability and validity of the measure with women with physical disabilities, including SCI (Taylor et al., manuscript in preparation). Furthermore, our results support the diagnostic value of somatic symptoms when assessing depression among women with physical disabilities, suggesting that somatic items should not be removed from the BDI-II when screening for depression among women with SCI and other physical disabilities.
We are pleased that TIRR Memorial Hermann is committed to addressing both the physical and psychological health needs of women with disabilities. To address depression, anxiety and other mental health issues among community-residing men and women with SCI and other disabling conditions, TIRR Memorial Hermann offers inpatient and outpatient psychotherapy services. The rehabilitation hospital’s commitment to the unique needs of women with disabilities is visible in its long-term affiliation with Hunter Hamill, MD, and the recent appointment of Terri Samuels, MD, both urogynecologists with expertise and experience providing clinical services to women with physically disabling conditions, including SCI. The TIRR Memorial Hermann SCIDR has also recently joined forces with Margaret Nosek, PhD, founder and director of the Baylor College of Medicine Center for Research on Women with Disabilities, to collaborate actively on research projects focused on the health and wellbeing of women with SCI and other disabilities. In addition, Dr. Taylor has recently formed a new Task Force on Women with SCI as part of the American Congress of Rehabilitation Medicine’s Spinal Cord Injury – Interdisciplinary Special Interest Group (ACRM SCI-ISIG), with Dr. Robinson-Whelen and Lisa Wenzel, MD, attending physician in the Spinal Cord Injury and Specialty Rehabilitation Programs at TIRR Memorial Hermann, serving as founding members of the task force. The synergy from these activities and collaborations will allow us to continue to expand the knowledge, research and clinical services we make available to women with SCI and other disabilities.
References
Arango-Lasprilla JC, Ketchum KM, Starkweather A, Nicholls E, Wilk AR. Factors predicting depression among persons with spinal cord injury 1 to 5 years post injury. NeuroRehabilitation 2011;29:9-21.
Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. 1996. San Antonio, Texas, Psychological Corporation.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: A systematic review. Spinal Cord. 2009;47:108-14.
Fann JR, Bombardier CH, Richard JS, Tate DG, Wilson CS, Temkin N. Depression after spinal cord Injury: Comorbidities, mental health service use, and adequacy of treatment. Archives of Physical Medicine and Rehabilitation. 2011;92:352-60.
Hughes RB, Swedlund N, Petersen N, Nosek MA. Depression and women with spinal cord injury. Topics Spinal Cord Injury Rehabilitation 2001;7(1):16-24.
Kalpakjian CZ, Albright KJ. An examination of depression through the lens of spinal cord injury: Comparative prevalence rates and severity in women and men. Women’s Health Issues. 2006; 16:380-388.
Krause JS, Kemp B, Coker J. Depression after spinal cord injury: Relation to gender, ethnicity, aging, and socioeconomic indicators. Archives of Physical Medicine and Rehabilitation. 2000;81:1099–1109.
Krause JS, Broderick L. Outcomes after spinal cord injury: Comparisons as a function of gender and race and ethnicity. Archives of Physical Medicine and Rehabilitation. 2004;85(3):355-62.
Krause JS, Brotherton SS, Morrisette DC, Newman SD, Karakostas TE. Does pain interference mediate the relationship of independence in ambulation with depressive symptoms after spinal cord injury? Rehabilitation Psychology. 2007;52(2):162-69.
Post MWM, van Leeuwen CMC. Psychosocial issues in spinal cord injury: A review. Spinal Cord. 2012;50:382-89.
Robinson-Whelen S, Taylor HB, Hughes RB, Nosek MA. Depressive symptoms in women with physical disabilities: Identifying correlates to inform practice. Archives of Physical Medicine and Rehabilitation. 2013;94:2410-16.
Robinson-Whelen S, Taylor HB, Hughes RB, Wenzel L, Nosek MA. Depression and depression treatment in women with spinal cord injury. Topics in Spinal Cord Injury and Rehabilitation. 2014;20(1):23-31.
Taylor HB, Robinson-Whelen S, Swank P, Hughes RB, Nosek MA. Factor structure of depression among women with physical disabilities. Manuscript in preparation.
Woolrich RA, Kennedy P, Tasiemski T. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychology, Health & Medicine. 2006;11(1):80-90.
Heather B. Taylor, PhD, is director of spinal cord injury research at the Spinal Cord Injury and Disability Research Center (SCIDR) at TIRR Memorial Hermann, and an assistant professor in the department of Pediatrics with adjunct appointments in the departments of Physical Medicine and Rehabilitation at McGovern Medical School at UTHealth and Baylor College of Medicine. Susan Robinson-Whelen, Ph.D., is an investigator at the SCIDR, senior investigator at the Center for Research on Women with Disabilities and an assistant professor in the department of Physical Medicine and Rehabilitation at Baylor College of Medicine.
