The specialists of the Memorial Hermann Hip Fracture Program are dedicated to providing the highest quality care to you and your family member(s). Our evidence based treatment plan is based on standardized protocols resulting in expedited care that appropriately addresses your clinical condition. Our goal is to minimize the time you are in pain, prevent complications commonly caused by lack of mobility, including bed sores, blood clots and pneumonia, and to ensure that you remain an active participant in your care experience. An unexpected incident resulting in a broken bone is a frightening event. We want you to feel confident that you are in excellent hands. Our affiliated physicians, nurses and therapists are experienced, compassionate, and ready to put their specialized skills and training to work in caring for you.
Our Program
- Cares for thousands of hip fracture patients every year using a variety of surgical and nonsurgical techniques.
- Is led by surgeons who are board certified and fellowship trained.
- Employs a multidisciplinary team approach to caring for you and your family.
- Utilizes resources and specially trained staff dedicated to the care of hip fracture patients.
An important goal of our specialized hip fracture program is an early effective pain control and medical/ surgical intervention, which leads to the best possible result for you. This guide will assist you in understanding what to expect following a hip fracture, including available treatments, possible complications and recovery.
What to Expect
After a hip fracture, patients typically arrive at Memorial Hermann through the Emergency Department or are admitted directly from a nursing or assisted living facility. The diagnosis of a hip fracture usually occurs in the Emergency Department following a review of your medical history and physical examination. You will be evaluated first by the Emergency Department physician and receive a series of blood tests and X-rays. It is important that the physician be advised of any other medical problems you have so that treatment of the hip fracture can begin immediately, including any medications you are taking (especially if you are taking any anticoagulant medication (e.g., Xarelto, Eliquis, Savaysa, Pradaxa, Coumadin, Plavix, etc.)). Information from this examination will be used to help evaluate your overall physical condition and treatment plan. Additional tests may be ordered based upon your individual condition to assess your overall health.
As quickly as possible, an anesthesiologist will evaluate you and take steps in order to manage the pain you will be experiencing, and a hospitalist will continue your treatment by making sure you are medically stable and prepared for surgery. Once the care team is sure that you are stable, a decision concerning the treatment of the fracture can be made and one of the experienced orthopedic surgeons will repair the broken bone.
Introducing Your Health care Team
The experienced team at Memorial Hermann will focus specifically on you and your family. Do not be afraid to ask questions. This is a stressful time and we want to make this experience as pleasant as possible. Members of your health care team may include:
Orthopedic Surgeon - The physician who will repair your broken hip and oversee your care in the hospital and during follow-up.
Program Navigator - The navigator is a registered nurse who will serve as your coordinator of care throughout your stay. He or she will follow you throughout your stay and help you prepare for the transition when you leave the hospital. He or she also will answer any questions you or your family may have.
Anesthesia Provider - The physician who is responsible for managing your pain before and after surgery, as well as administering medications to keep you asleep and comfortable during your operation.
Hospitalist - A physician who may follow your medical care during your hospital stay and will work with your orthopedic surgeon to meet your care needs, including ensuring you are medically prepared for surgery.
Cardiologist - If you have a history of heart disease, a cardiologist may see you prior to your surgery to assess your condition. The cardiologist may also assist in managing any heart medications you may need throughout your hospitalization and recovery.
Case Managers - These team members help to plan your transition from the hospital to your home, or other setting of care, and arrange for any additional equipment and services needed.
Nursing Team (Registered Nurse, Licensed Vocational Nurse, Patient Care Assistants) - Before, during and after your surgery, you can expect to meet different nurses who perform many different jobs. Nurses will help prepare you for surgery and will be in the operating room with you throughout your surgery. After surgery, the nursing team will carry out all orders given by your team of physicians, as well as keep you comfortable and safe in the hospital.
Physical Therapist - Your physical therapist is trained to help you gain strength and motion after your surgery and will help ensure that you do your exercises correctly. Your physical therapist will also help teach you how to properly and safely use your walker.
Occupational Therapist - Your occupational therapist is trained to help you learn to safely and effectively perform activities of daily living, such as bathing and dressing. The occupational therapist will also teach you how to use special equipment, such as long-handled reachers or shower seats, which you may need during your recovery.
Dietitian - Your dietitian provides nutritional counseling to help you make healthy choices about the foods you eat and helps you understand the connection between diet and healing.
Other team members that you may meet include pharmacists, lab and X-ray technicians, patient transporters and respiratory therapists.
About Hip Fractures
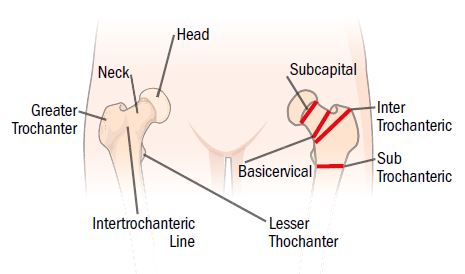
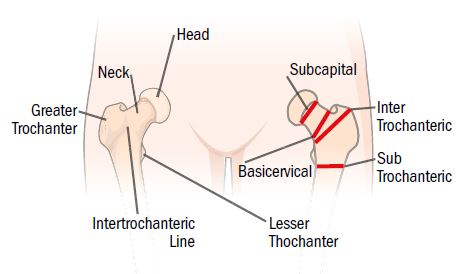
The top of your femur is categorized into four main parts: the subtrochanteric region near the bottom of the hip joint, the intertrochanteric region in the middle of the joint, the greater trochanter at the top of the joint, and the femoral neck that connects the femur to the femoral head. Hip fractures occur in three main areas: femoral neck, intertrochanteric region, and subtrochanteric region.
The type of surgery you have depends largely on where your fracture has occurred. The following describes these different types of hip fractures and some common procedures to repair them.
Femoral Neck Fracture
What is it?
In this type of fracture, the ball is essentially broken off of the femur, which is also known as the thighbone. With a femoral neck fracture, there is a chance that the blood supply to the ball of the hip will be interrupted. In most cases, this will need to be fixed in surgery.
How is it fixed?
Depending on how stable the fracture is will depend on what type of treatment is needed. Two of the more common treatments are: hemiarthroplasty (half of a hip replacement), or metal pins or screws. A third option may be a total hip replacement.
- Hemiarthroplasty – This is when the broken ball of the hip is replaced with an artificial metal ball. In this case, there is nothing wrong with the socket and it is left alone.
- Metal pins or screws – This treatment is used when the fracture is more stable. The pins, or screws, are used to keep the fracture stable.
- Total Hip Replacement – This treatment may be necessary if you also have some arthritis in your hip. Both the ball and the socket would be replaced.
Intertrochanteric Hip Fracture
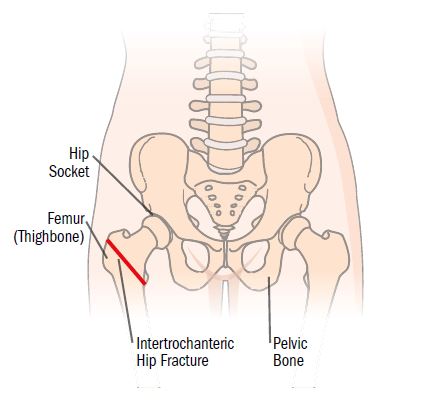 What is it?
What is it?
An intertrochanteric hip fracture may be described as a break through the top of the femur, or thighbone. This type of fracture occurs just below the neck of the femur. In most cases, this fracture will not be stable and will need to be fixed in surgery.
How is it fixed?
The way this fracture is fixed depends on the stability of the fracture and also the surgical recommendation of the surgeon fixing the fracture. Two of the more common ways to fix this fracture include:
- A metal rod or nail – A long metal rod or nail is inserted into the canal of the bone. At the top of the nail, or rod, is a place for a screw. This screw will help keep the bone compressed and in place as the bone heals.
- A metal compression screw – A plate is inserted along the side of the femur and several screws are used to hold the fracture in place. One main screw will allow the fractured bone to compress as the bone begins to heal.
Subtrochanteric Hip Fracture
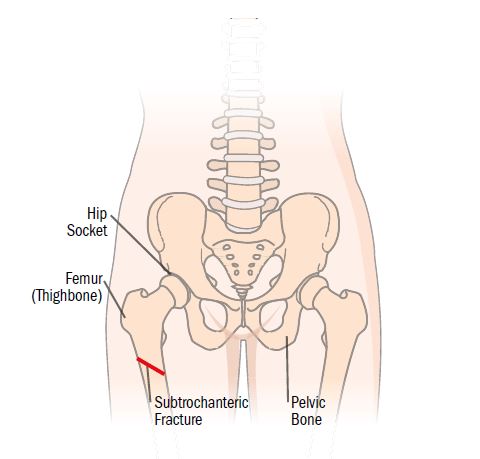 What is it?
What is it?
This fracture can be described as a break across the shaft of the femur. These fractures usually are not stable and require surgery to stabilize the fracture.
How is it fixed?
There are several different ways that this fracture can be fixed. The way it is fixed depends on the stability of the fracture and also the preference of the surgeon. One of the more common ways to fix these fractures is:
- A metal rod or nail – A long metal rod or nail is inserted in to the canal of the bone. At the top of the nail, or rod, is a place for a screw. This screw will help keep the bone compressed and in place as the bone heals.
Other Fragility Fractures
Pelvic Fractures
The pelvis is the bony ring structure that attaches your lower extremities to the spine. It also holds the cup portion of the hip joint called the acetabulum. Both the ring and acetabulum may break when you experience a fracture.
Pelvic ring fractures may be stable, which means that the fracture pieces will not move, or unstable, which means the pieces will be able to move and cause pain and heal in a crooked position. The treatment depends on the fracture stability. The stable fracture is able to withstand the forces of weight bearing and you will be mobilized. The unstable fracture requires stabilization of the fragments by long screws or plates inserted through small incisions using a special X-ray machine that allows your surgeon to see what is happening.
Shoulder Fractures
Fractures of the proximal humerus involve your shoulder joint. Because the shoulder joint has a great range of motion, the need for an exact reduction is not necessary as you regain all the motion you need for normal function with nonoperative care. However, in situations where the fracture is severely displaced, operative treatment will be recommended to assure healing and function. These fractures are usually fixed with metal plates and screws. However, if the surface of the joint is involved or the number of pieces is excessive, replacement of the shoulder may be performed.
Implant-Related Fractures
Many people have had a hip or knee replacement done for the treatment of their arthritis. With weaker bone there is a potential for the bone to fracture about the implant. As most joint replacements are done in the hip and knee, it is very common for the femur to be the site of these fractures. Based on the amount of involvement of bone near the prosthesis and the need for you to be mobilized, the treatment of theses fractures ranges from metal plate or nail fixation of the fracture to redoing the joint replacement.
In the Hospital
From the moment you arrive at the hospital until after surgery, you may not be allowed to eat or drink. This will reduce the risk of complications during your surgical procedure. An IV will be inserted to keep you hydrated, and you will be given antibiotics to help prevent infection. For your safety, you will remain in bed until after surgery. A urinary catheter may be inserted to drain your bladder. In order to prevent blood clots, you may be placed in foot or leg pumps and compression stockings. To help prevent pneumonia, you may be given a small device called an incentive spirometer to help improve your deep breathing. After surgery, you will be given a medication to help in the prevention of blood clots, which will continue for a few weeks after the surgery.
Managing Your Pain
Managing your pain safely and effectively is important to us. A fractured bone can be very painful, especially before surgery. There are many new pain management techniques used by the Memorial Hermann Hip Fracture Program to manage your pain and make you as comfortable as possible.
Your health care team will do everything possible to decrease your discomfort using medications and other techniques; however, you should not expect to be totally pain free.
If you are having pain, please report it to your caregiver immediately. Do not wait until your pain is unbearable before asking for pain medications. Treating pain early is easier than treating it after it has become severe. You can help your health care team "measure" your pain. While you are recovering, your health care team will often ask you to rate your pain on a scale from 0 to 10. Using this scale to measure your pain helps the team know how well your treatment is working. Our goal is to not let your pain reach a level above 5-6 on the pain scale.
Managing a Safe Environment
During your hospital stay, we want to ensure your surroundings are safe and prevent any activity that could increase your risk of re-injury, including falling. A yellow bracelet will be placed on your wrist to alert the staff and members of your family that you are at risk for a fall. Always use your call light for assistance to get out of bed with hospital staff, not family. Further safety measures may include the use of bed alarm, chair alarm, safety belt and frequent checks by nursing staff to ensure that special attention is provided for your needs and welfare.
Managing a Quiet Environment
We will make every effort to limit nighttime interruptions as much as possible. Please understand that we will be checking on you during the night to make sure you are okay. Sometimes it will be necessary to wake you up during the early morning hours for routine checks and blood tests that your physician has ordered. These normal procedures are to ensure that your physician has the results available as early as possible.
Managing Possible Complications
Complications can occur after a hip fracture and, generally, are related to immobilization. The most common complications are:
- pneumonia
- pressure ulcers (bed sores)
- blood clots or thrombophlebitis
- mental confusion (delirium)
- urinary tract infections (UTIs)
Getting out of bed and moving can reduce the risk of developing these complications. If an operation is necessary to stabilize your fracture, your health care team will assist you with getting up as soon as possible to help reduce the overall risk of developing these complications.
Pneumonia
Bed rest can increase the risk of developing pneumonia in older patients. If anesthesia is required for surgery, the risk is even greater. After any injury that requires bed rest, you will need to do several things to keep your lungs working their best. Your nurse will coach you to take deep breaths and cough frequently. Getting out of bed, even upright in a chair, allows the lungs to work much better. As soon as possible, you will be allowed to sit in a chair.
The incentive spirometer is a small device that measures how hard you are breathing and gives you a tool to improve your deep breathing. If you have any other lung disease, such as asthma, the respiratory therapist may also use medications that are given through breathing treatments to help open the air pockets in the lungs.
Pressure Ulcers (Bed Sores)
Hip fractures cause pain when you move, even in bed. As a result, you stop moving around to shift your weight from time to time as you normally would. If something prevents you from shifting and the pressure stays constant in one area, that area of skin may eventually become damaged due to lack of blood flow. This damage is called a pressure ulcer or bed sore.
The best treatment is to prevent bed sores in the first place. Nurses routinely assist to move patients in bed every few hours to make sure the skin is not getting too much pressure in one area. The best way to prevent pressure ulcers is to get you out of bed and moving when possible.
Blood Clots
Blood clots, sometimes called deep venous thrombosis (DVT), can result from bed rest and inactivity. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots break apart, they can travel to the lungs and cut off the blood supply to a portion of the lungs. This is a life-threatening condition called pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the blood vessels.)
There are many ways to reduce the risk of DVT, but the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include:
- Leg pumps or foot pumps with pressure stockings to keep the blood in the legs moving
- Medications that thin the blood and prevent blood clots from forming
Mental Confusion (Delirium)
Aging adults who suffer a hip fracture and go to the hospital are under a lot of stress. Unfamiliar surroundings, pain medications, and the stress of the injury can lead to changes in a patient’s behavior. This sometimes seems to get worse at night and it can be very frightening to both patients and their families. Fortunately, it is almost always temporary.
The best treatment for mental confusion is usually to get patients moving and out of the hospital, and to avoid the use of narcotic pain medication. Familiar surroundings, familiar faces, and activity are the best treatments. Medications are used when necessary. Again, this is usually temporary and will resolve in time.
Nutrition
Studies have shown that many older patients can be malnourished and that taking a protein supplement with calcium can help avoid complications. Protein, vitamin C, and vitamin D aid in the healing process of your cells, and calcium is needed to build and strengthen bone. You will be given this supplement to drink while in the hospital. Our dietitian will assist you in planning menu choices to ensure you have the proper diet.
Osteoporosis
Osteoporosis is the thinning of bone tissue and loss of bone density over time. This occurs when the body fails to form enough new bone, when too much old bone is reabsorbed by the body, or both. Some risk factors include:
- age
- menopause
- family history of osteoporosis
- smoking
- eating disorders
- low body weight, too little calcium in the diet
- heavy alcohol consumption
- medications such as steroids and anticonvulsants
Unfortunately, there are no early symptoms of osteoporosis. Fractures of the vertebrae, wrists, or hips may be your first clue you have osteoporosis. Bone pain, tenderness, loss of height and stooped posture are late symptoms.
There are several tests that can be performed to evaluate for osteoporosis such as a DEXA scan, X-rays or measurement of the calcium in your urine. As for treatment options, there are several ways to handle this disease. Physical exercise can reduce the chance of fractures associated with osteoporosis. Weight-bearing exercises such as balancing exercises, stationary biking, rowing machines, walking and jogging are some of the examples. A diet that includes an adequate amount of calcium, vitamin D, and protein should be maintained. Foods rich in calcium include milk, yogurt, cheese and salmon. If you have been told you have osteoporosis during this hospitalization it will be important to have follow-up care for this condition. Our health care team will assist you with this follow-up.
Managing Constipation
Taking narcotics for pain management or other medications may result in constipation. It is highly recommended to increase fluid intake, eat foods high in fiber, and increase mobility. Intake of a bran mixture of 3 cups unsweetened apple sauce, 2 cups coarse wheat bran, and 1½ cups unsweetened prune juice significantly reduces laxative use. Other sources of fiber are fruits, vegetables or nuts. Your physician may order medications to help with constipation if high fluid intake and a high fiber diet are still not helping.
After Surgery
Therapy Goals
Hip surgery can affect your ability to move around, as well as normal daily activities. This is likely one of the most frightening and painful experiences that you or your family member has experienced. It is unplanned and usually takes everyone off guard. In addition to your medical team of physicians and nurses and many others, your therapists will assist you during your hospital stay and return you to the highest level of function possible.
Our goals for you/your family member are to:
- Move – with the help of therapy – as soon as medically stable and appropriate as determined by your orthopedic surgeon – likely on the day of surgery or within 24 hours of your surgery.
- Have adequate and consistent pain management to participate at the highest functional level possible. You will not be pain free, but the more you move the better your hip will feel.
- Be able to safely get up to the edge of your bed, get to a bedside chair and a bedside commode.
- To be able to walk with the assistance of a walker (or other equipment as appropriate).
- Perform your activities of daily living, such as grooming, dressing, toileting and showering.
- For those patients with hip replacements, communicate understanding of hip precautions and be able to integrate them into activities of daily living.
Participation in Therapy
In order for you to return to your highest level of function as quickly as possible, it is imperative that you have adequate pain control to be able to move around throughout the day. Typically if you do not move, you may not hurt too badly and not request or get pain medicines. When you may have to get up to the bathroom or participate in therapy, the pain increases quickly and intensely. The solution to this problem is to have pain well controlled throughout the day so that you are able to handle a small amount of pain during activities, without needing heavier doses of pain medications. This means taking medication consistently throughout the day and night that will allow you to move. This ability to move also helps to alleviate other complications previously described in this book.
Weight-bearing Status
Depending on the type of surgery you have to repair your hip and your surgeon’s preference, the amount of weight you can put on that leg may be limited.
- Weight bearing as tolerated - You can put as much weight on your leg as you can tolerate.
- Partial weight bearing - Less than 50% of your weight on your operative leg.
- Touch down weight bearing - Only allowed to put your toes down on operative leg to balance; VERY minimal weight bearing.
- Non-weight bearing - Not able to bear any weight on operative leg.
Hip Precautions
Limit Leg Lifting
Do not prop or lift leg up past 90 degrees at affected hip.
Some activities such as cutting toenails or shaving legs will require assistance from others.
No Adduction
Keep legs apart at all times. do not cross legs whether standing, sitting or lying down. Use pillow to keep legs apart in bed.
No Internal Rotation
Do not twist affected leg inward. Keep foot pointed forward or out to side. This also applies when lying in bed. May use towel roll to keep leg from rolling inward.
Total and Partial Hip Precautions Only
- No bending of your hip more than 90 degrees. Knee should be below hip and shoulders behind hip at all times.
- No crossing the middle of your body with operative leg.
- No turning the operative leg inwards. No toes inward.
Exercises
Your physical therapist will begin with personalized exercises with you to not only help move the hip, but also to increase your strength and range of motion in your hip. You should be performing the exercises given to you twice a day.
Preventing Future Injury
After you recover from a fracture the last thing you want to do is endure another injury, and falls are the most common way to re-injure a hip. Falls can be caused by loss of balance, medication side effects, poor vision, impaired mobility, or environmental problems.
You can prevent a fall by following the below guidance:
Stairways
- Make sure all handrails are not broken and are securely fastened.
- Both sides of the steps should have handrails.
Floors and Rugs
- Remove rugs and runners that tend to slide
- Secure all rugs, including area rugs, to the floor
- with tacks, non-skid pads or double-sided tape.Ensure all floor boards are even.
- Use non-skid floor wax.
Bathroom
- Use non-skid mats in the tub and shower and on the bathroom floor.
- Add a bath or shower seat if you are unstable when standing
- Never use a towel rack or soap dispenser/dish for support as these can easily come loose, causing you to fall.
- Attach grab bars to structural supports in the wall or install bars specifically designed to attach to the sides of the bathtub.
- Remove soap buildup in tub or shower on a regular basis.
Kitchen
- Items that you use frequently, such as dishes, should be easy to reach.
- Ensure that your step stool has a handrail that you can hold when climbing on the top step, and all screws and braces are tightened and secured.
- Discard stools with broken parts.
Lighting
- Use maximum wattage bulb allowed by the fixture (if you’re unsure, do not exceed 60 watts).
- Place nightlights in hallways, bedrooms, bathrooms, and stairways.
- Install light switches at the top and bottom of stairs.
- Place a lamp (and telephone) near your bed.
- Keep lighting uniform in each room and add lighting to dark spaces.
- Keep a working flashlight in a convenient location at the bottom and top of stairwells and close to your bed in case electric power goes out.
All Rooms
- Arrange furniture so that outlets are available for lamps and electric appliances without use of extension cords.
- Check whether hallways and rooms have obstacles to safe movement.
- Move newspapers, boxes, electrical and phone cords, plants and furniture out of traffic areas.
- Store clothing, bed coverings, and other household items where you can reach them comfortably.
- Keep a telephone close to your bed for emergencies.
Outside of Your Home
- Repair holes, uneven joints on walkways.
- Be cautious of any surfaces that may be slippery. Arrange to have wet leaves removed from stairs and walkways.
- Make sure outside lighting is working in entryways and other walk areas.
- Check that handrails are not broken and are securely fastened. Both sides of steps should have handrails.
Other Essential Steps for Protecting Yourself Against a Fall
- Assess your home to identify fall hazards and make the necessary changes to prevent them.
- Ask your physician or pharmacist about the effects of the prescription and non-prescription medications you are taking. Some medications can cause dizziness or lightheadedness that can lead to falls. As people age, the effects of medications may change.
- Have your eyes checked every year. Vision problems can cause falls.
- Check with your physician about appropriate physical activity and exercise. Stay as physically active as you can. Exercise helps to prevent falls, especially activities that enhance balance and coordination.
- Be careful to wear shoes that do not cause you to trip. The soles should be non-slip and not too thick.
Discharge Instructions
Call the office if you develop any of the following:
- Persistent bleeding.
- Persistent nausea/vomiting.
- Numbness, tingling, discoloration, loss of sensation of affected extremity.
- Fever greater than 100.4 degrees fahrenheit/chills/dizziness.
- Redness, swelling, or pus in surgical incision.
- Pain, swelling, or redness in calf.
- If your cast or splint becomes wet or too tight.
- Any unusual symptom that doesn’t seem right.
Diet
Resume diet as tolerated. Drink plenty of water and other fluids.
Activity
- Weight bearing.
- Weight bearing as tolerated (WBAT): You can walk on the injured limb with as much weight as you like. If it hurts too much, then try partial weight bearing and slowly increase it to full weight.
- Touchdown bearing: you can rest your foot on the floor so you don’t have to hold it in the air. But now weight can actually be placed on the limb.
- Elevate injured limb ABOVE the heart to help swelling improve.
- Use assistive devices, such as a wheelchair, walker, crutches, or cane as instructed.
- Pump your ankles up and down at least 20 times per hour to help prevent blood clots
Incision/Dressing
- In most circumstances, when you leave the hospital, you can start to shower and let water run over the incisions. Do not submerge or soak the wounds in water such as a bath or swimming pool.
- DO NOT touch or scratch your incision.
- DO NOT put ointments of any kind on your incision.
Ice
Place a towel over the splint/extremity. Apply a large bag of ice to the operative site for 30 to 45 minutes every 2-3 hours. Continue to ice as needed to control pain and swelling as you become more active.
Pain
Pain is normal and expected after surgery. You will not be pain free. Take pain pills only as prescribed for as long as needed. Pain medication can cause constipation. Drink plenty of fluids and eat high fiber foods. If needed, the following over-the-counter remedies are recommended: Senakot, Colace and Milk of Magnesia.
Miscellaneous
Have a responsible adult with you for approximately 24 hours following surgery. We recommend that you do not make any critical decisions, sign any legal papers or operate any dangerous equipment for 24 hours following surgery or while taking prescription medicines.
Follow-Up
Please bring a list of all current prescriptions to each follow-up appointment. If the patient is not able to communicate or make medical decisions, please have a family member accompany him or her. Typical follow-up is as follows:
- 2-3 weeks: suture removal, wound check and pain assessment
- 6-8 weeks: X-rays for bone healing, range of motion and pain assessment
- 10-12 weeks and every 2-3 months thereafter until healed for X-rays to assess healing, range of motion and function.
Language Resources
Interpreter services, including American Sign Language, are available 24 hours a day to provide or arrange for interpreters to assist patients and staff members. If you require an interpreter, please ask a staff member to arrange one for you.
Individual Rights
Access: You have the right to review or receive a copy of your medical information, with limited exceptions. You may request that we provide copies in a format other than photocopies. We will use the format you requested unless we cannot practicably do so. If we maintain your medical information in an electronic format, you may request and we shall provide you with the requested information in an electronic format. You must make a request in writing to obtain access to your medical information. You may obtain a form to request access or a copy of your medical information from memorialhermann.org webpage and mail the completed form to Memorial Hermann Release of Information, 7737 SWF C94, Houston, Texas 77074 or the Release of Information Department, located at the facility where you obtain your medical care.
There is a charge for a copy of your medical information.
Medical Records
The Memorial Hermann Release of Information department is dedicated to processing your requests for patient-protected health information in a timely manner, while maintaining patient confidentiality. Hours of operation are Monday through Friday from 8 a.m. to 4:30 p.m. For your convenience, we have one central mailing address for all Memorial Hermann hospitals and outpatient centers:
Memorial Hermann Release of Information
7737 SWF C94
Houston, TX 77074
Additional information can be found online by accessing the Patient & Caregivers tab at www.memorialhermann.org.
Paperwork
Injury that causes a change in your daily activities brings with it paperwork that must be completed within a timely manner. You are responsible for obtaining paperwork and getting it to our office to be completed. While we make every attempt to complete paperwork as quickly as possible, we do require 5 business days to do so. It is not possible to complete paperwork during a clinic visit. All paperwork requires that the patient fill out a portion that includes a signed release of information statement. If the paperwork is faxed directly to the office, your legal name and birth date must be included. It is also a good idea to call the office to make sure that faxed paperwork was received.
- Work/School excuse: These are provided during clinic visits upon request.
- FMLA: This will come from your employer. It may be for the patient or a family member who will be a care provider. If it is faxed directly to the office, be sure to clearly indicate the patient's full name and date of birth on the form.
- Disability: Paperwork will come from your insurance company. If faxed to the office, be sure to clearly indicate the patient’s full name and date of birth.
- Medicaid: If you do not already have a Medicaid member number, you must apply through the Social Security office. If you will require transportation assistance through Medicaid, you must apply for it 5 days prior to the needed date.
- Workers' Compensation: This is initiated through your employer. You will be provided a case number and be assigned a case worker. Our office will work closely with you and your caseworker during your treatment and follow-up.
Medications
How to rate your pain: You will be asked to rate your pain using the 1 to 10 pain scale, with one being no pain to 10 being the worst pain imaginable. You will also be asked to qualify your pain, using terms like sharp, dull, throbbing, burning or aching. Please note that you will not be pain-free. The goal is to make the pain tolerable. Please refer to "Wong-Baker Faces Pain Rating Scale" on page 10.
Prescription Pain Medicine: Hydrocodone is the most common narcotic medication used for surgical pain. Oxycodone is more rarely used for severe pain. Both hydrocodone and oxycodone cannot be called into your pharmacy; they require a special written prescription. You may be prescribed these narcotic pain medicines for up to 6 – 12 weeks, depending on your pain requirements. If more potent pain medicines are required during these initial weeks or if pain medicine is required beyond 12 weeks, you may be referred to another physician who specializes in pain management. Never take more of these medicines than prescribed because you are having more pain. If your pain is not rating a 4 or lower on a scale of 1-10 and you are elevating, resting and icing, call the nurse. Do not attempt to drive or operate machinery while taking narcotic pain relievers.
Non-narcotic Pain Control
Neurontin (gabapentin): This prescription medicine is used to treat nerve pain, which is a burning pain that some patients experience after surgery. Gabapentin needs to be “stepped up” and "stepped down,” meaning that you gradually increase your dose over time and gradually decrease your dose when you stop taking it. For elderly patients, you may start at a lower dose, which is 100mg three times a day. Generally, you will start with 300 mg the first day, then 300 mg twice a day on day 2, and 300 mg three times a day until you stop taking it. When you are stopping this medication, you will go to two times a day the first day, then 300 mg on day two, and none the following day. The dose of gabapentin may be increased by your physician. Keep in mind that this medication must be taken as directed, and cannot be taken on an as-needed basis.
Ultram (tramadol): This prescription medication may be prescribed when you are transitioning from narcotic pain medicine to over-the-counter pain medicine or other narcotic medicines. It also is prescribed in addition to other medicines, working synergistically to reduce your pain. Do not take tramadol if you have a history of seizures, and notify your physician if you are taking prescription medications for depression, as this medicine may not be appropriate for you.
Tylenol (acetaminophen): This medication is available over the counter. It is non-narcotic and not sedating. It is very effective, particularly in elderly patients. You can take it every 6 hours, but do not take more than 4 grams per day in total.
Blood Clot Prevention
- For the first 3-4 weeks after surgery, you likely will take medicine to help prevent blood clots. These include aspirin, Lovenox (enoxaparin), Coumadin (warfarin) and a few others.
- Do not remain in the same position all day; walk as much as possible. If you are having difficulty walking, at least move from bed to chair 2-3 times per day.
- Actively pump your knees (straight and bent) and ankle (up and down) to help circulate blood flow and prevent blood clots.
Bone Health Medications
- Calcium: Take 1,500 mg of calcium a day, divided into three 500 mg doses taken with meals (over-the-counter medication).
- Vitamin D3 (cholecalciferol): Take 1,000-2,000 international units per day (over-the-counter medication).
- Vitamin D2 (ergocalciferol): You may be prescribed ergocalciferol if there is concern for a significant vitamin D level. If so, you will take 50,000 units ergocalciferol for about 2 months, in addition to daily over-the-counter calcium-vitamin D.
Important Information About Prescription Refills
- Notify your physician or his assistant as soon as possible when you need a refill. It may take up to 24 hours for your call to be returned.
- If you call after 5 p.m. on weekdays, do not expect a callback until the next work day. If you call after 5 p.m. on Friday, do not expect a callback until Monday morning. If you leave a message, you will be asked to speak slowly and spell your last name, and leave your date of birth and phone number. To expedite your request, leave the name and phone number of the pharmacy you choose.
- Ultimately, it is your physician’s decision whether to authorize a refill of pain medication. It is our goal to gradually decrease the strength and amount of pain medicine you take. This may take time, and your pain may increase for a short time when you become more active. This is normal and expected.
How can I help my bones heal?
- Avoid anti-inflammatory medicines: Studies suggest that ibuprofen and similar products, like Aleve, may inhibit bone growth, which may delay healing.
- Avoid caffeine: Caffeine increases the rate of calcium loss through urine, decreasing the amount that is available in your blood for bone building.
- Do not smoke: Patients who smoke experience a longer healing time and are at higher risk of nonunion (non-healing of the bone), wound problems, infection and chronic pain. Smoking (nicotine) causes vasoconstriction (blood vessels get narrower,) decreasing blood flow to the healing bones. Nicotine use is also associated with chronic pain.
- Avoid alcohol: Alcohol consumption interferes with the formation of new bone cells and should not be taken while using pain medication.
Physical Therapy
You may be given a prescription for physical therapy. You will take this prescription to the physical therapist of your choice. It is best to choose one close to home, as you will go several times a week. Let your therapist know when you have a clinic appointment, so you can bring progress notes with you.
Home Exercises
You may be given an instruction sheet with home exercises. While you are at home recovering from surgery, your homework is to work on your ankle. You have a lot of time. The more you work on the injury, the better it will get.
Going Back to Work
Returning to work depends on what kind of fracture you have and what kind of work you do. Some jobs require that you return to work with no restrictions, while others will allow you to return to work with provisions that allow you to continue healing while on the job. We will provide you with documentation explaining what you can or cannot do while on the job, and it will be up to your employer to accommodate your needs or have you remain off work until you are able to return to full duty without restrictions. For safety reasons, it is not appropriate to return to work while regularly taking narcotic pain medication.
Dentist and Antibiotics
It is only necessary to pre-medicate with antibiotics for the dentist if you have had a joint replacement. If you have had a joint replaced and are visiting the dentist, please call the office several days before your appointment so that your physicians can decide if you need to be treated and we can get it called into the pharmacy.
Travel and Hardware
You do not need any special identification to show at airport security relating to your hardware. In the past, identification cards were widely accepted, but today they are not. If you should set off the alarm, notify security officers where you had surgery. Most patients maneuver through airports with no problems whatsoever.
Equipment Needs
After this type of injury you will need an assistive device to help you walk, such as a rolling walker, a 3-in-1 commode, or tub transfer bench. For your safety, if you are walking with an assistive device in the home you should always be sitting for your bath/showers. Your needs will dramatically change between now and the time you go home. Your team will help you determine which equipment is most appropriate for you. The facility where you are discharged home from is responsible for ensuring you have the necessary equipment upon your discharge. Unfortunately, this bathroom equipment is not USUALLY covered by your insurance, so we recommend you look online for equipment or check local stores. You may also check with local churches or organizations that may have medical equipment that you can obtain at significantly reduced price.
If you or a family member has questions during your treatment by your health care team, do not hesitate to let us know. We are here to provide you the best care possible. Additionally, below are some answers to frequently asked questions related to your recovery.
Find Relief for Hip Pain
Each year, Memorial Hermann Joint Center physicians perform more than 3,000 hip and knee joint replacement procedures, more than are performed at any other hospital system in the Greater Houston area.
If you're experiencing symptoms of hip pain and are seeking relief, Memorial Hermann Joint Centers can help. Our orthopedists see patients with everything from minor knee pain that requires rest and self-care, to those with chronic, serious knee pain, requiring a targeting non-surgical or surgical treatment plan.
Let's get started.
Contact us to learn more about Memorial Hermann Joint Centers and pain-relief solutions. Submit the form below and the Memorial Hermann Joint Center navigator will reach out to answer your questions and help guide you down the path to a life with less pain.
